Primary Progressive Aphasia: Variants and Main Language Domains
- Authors: Akhmadullina D.R.1, Fedotova E.Y.1
-
Affiliations:
- Research Center of Neurology
- Issue: Vol 18, No 4 (2024)
- Pages: 68-75
- Section: Reviews
- Submitted: 30.11.2023
- Accepted: 08.12.2023
- Published: 06.12.2024
- URL: https://annaly-nevrologii.com/pathID/article/view/1067
- DOI: https://doi.org/10.17816/ACEN.1067
- ID: 1067
Cite item
Abstract
Language is one of the higher brain functions and the primary method of communication, so it plays a key role in human social functioning. Primary progressive aphasia, as a slowly progressive neurodegenerative disease with a clinical predominance of different speech and language disorders, is a promising model for a more detailed study of topographic distribution of language disorders. This review presents data on different clinical variants of primary progressive aphasia and the corresponding clinical and neuroanatomical correlates that have significantly expanded the modern understanding of the neural network language organization.
Full Text
Introduction
Primary progressive aphasia (PPA) is a group of neurodegenerative disorders characterized by predominantly progressive language impairment. PPA usually manifests at the age of 50–60 years and affects both men and women equally. In addition to language disorders, other cognitive, behavioral, and motor disorders may develop over time. However, aphasia is the most disabling symptom, at least during the first two years of the disease [1].
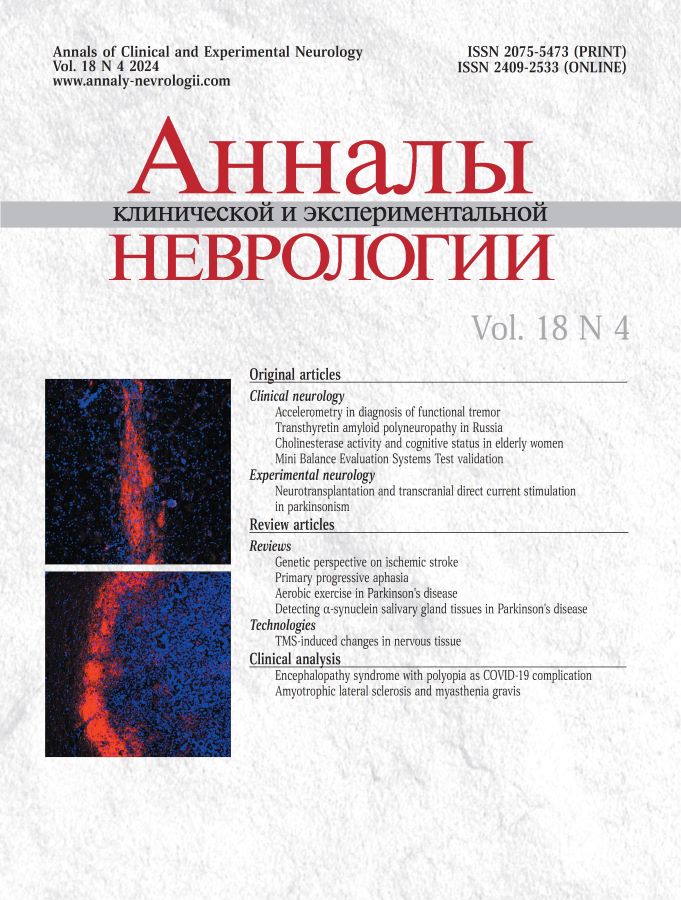
Neurodegenerative aphasia was first described by Arnold Pick in 1892 [2], but the term PPA was introduced only in 1987, when it was proposed to differentiate PPA from Alzheimer's disease (AD) as a distinct disease entity [3]. Initially, PPA was considered to be a single syndrome with a central symptom of anomia, but over time, three clinical syndromes have been identified such as non-fluent (nfPPA), semantic (svPPA), and logopenic (lvPPA) variants. This classification has been used since 2011, when the current diagnostic criteria for PPA were established, describing specific clinical and neuroimaging signs of each variant [1]. The Figure shows examples of PPA from the authors' clinical practice.
In recent decades, there have been significant advances in our understanding of the neurobiological mechanisms underlying language behavior and diseases that manifest with language impairment. At the same time, the study of PPA has played an important role in developing new concepts of language, initially and primarily based on studying stroke and other focal lesions. The localization of neurodegeneration and atrophy in PPA is unique and significantly different from the anatomical distribution of lesions in vascular disease. The speech deficits in PPA are also very diverse. Together, these findings identify novel correlations between brain regions and cognitive impairment and provide new directions for studying the neuroanatomical basis of language.
Non-fluent variant
NfPPA is characterized by apraxia of speech and agrammatism with relatively preserved understanding of single words and functions of objects [1]. Patients' speech becomes laconic and interrupted, with frequent stumbling, fluctuating rate, and decreased speaking activity. Patients with this variant tend to use simple sentences with minimal words. Spoken language understanding is less affected.
Neuroimaging of nfPPA is primarily characterized by atrophy of the left posterior frontal/insular regions (Figure, А), although the process starts affecting other brain regions over time [1, 4]. NfPPA usually develops in patients with frontotemporal degeneration, more commonly with 4R tau inclusions, less commonly with 3R tau or TDP-43, while up to 10% of cases may have an atypical presentation of AD [5, 6]. A positive family history is reported in one third of cases. There are nfPPA cases with mutations across all three major frontotemporal dementia genes such as C9orf72, MAPT, GRN [6].
Atrophy localization in primary progressive aphasia variants.
A — non-fluent variant (patient age 49 years, disease duration 5 years); B — semantic variant (patient age 72 years, disease duration 6 years); C — logopenic variant (patient age 64 years, disease duration 4 years).
The most characteristic areas of atrophy for each of the variants are outlined in red.
Agrammatism is characterized by misused prepositions, inconsistent endings or verb forms. This affects not only the grammatical structure of single words, but also that of sentences that are misconstrued by using nouns instead of adjectives, participles, or verbal adverbs. As the disease progresses, patients start using more laconic sentences and eventually develop so-called telegraphic speech. Agrammatism is found in both spoken and written language and include transposed letters and syllables, incorrect use of endings, and joined-up spellings of prepositions. Despite preserved comprehension of isolated words, patients have difficulty understanding syntactically complex structures such as passive voice or complex sentences [6]. Overall speech rate is reduced by more than 3 times compared to healthy controls [7].
Apraxia of speech is associated with poor complex motor planning and manifests as a disruption in speech rhythm and intonation. The disorder is most evident when people are asked to repeat a complex word or a phrase several times; people with apraxia repeat the word or phrase differently each time. The nfPPA is often associated with hypokinetic or mixed hypokinetic-spastic dysarthria [8]. It should be noted that in addition to nfPPA, there is a condition called primary progressive apraxia of speech (PPAS), in which patients present with an isolated apraxia of speech. In PPAS, apraxia of speech is the only manifestation without signs of aphasia, which is the main feature that distinguishes it from nfPPA. However, in some cases PPAS may progress to nfPPA over time.
In addition to language disorders, the clinical picture may include motor, behavioral, and other cognitive disorders. In nfPPA, behavioral disturbances occur less frequently and later than in other types of PPA, but symptoms such as apathy, agitation, depression, reduced empathy, eating disorders, and disinhibition may develop over time [9, 10]. Among non-speech cognitive impairments, impaired regulatory functions are more typical for nfPPA, with memory and visuospatial functions remaining intact for a long time [6].
Atrophy in nfPPA most commonly affects the opercular part of the left inferior frontal gyrus and left premotor cortex, with possible involvement of associated cortical and subcortical regions such as the anterior insula, prefrontal cortex, supplementary motor area (SMA), basal ganglia and supramarginal gyrus [1, 10].
In addition, nfPPA is characterized by the involvement of the left inferior frontal gyrus, which plays an important role in regulating the motor-phonological network and ensuring the correct use and comprehension of grammatically or syntactically complex structures in spoken and written language. Atrophy of this region correlates with the overall severity of aphasia and agrammatism in patients with nfPPA [11–13]. In addition to the left inferior frontal gyrus, the severity of agrammatism and aphasia in nfPPA is also associated with damage to thalamus and putamen [11], while a decrease in fluency is associated with the volume of the anterior insula [14].
In contrast to agrammatism, apraxia of speech most often correlates with damage to the left premotor cortex and SMA. The SMA plays a role in movement initiation and speech motor control, and its atrophy is associated with reduced articulation rate in PPA [15]. The left superior lateral premotor cortex is involved in planning complex actions and is thought to determine the sequence of syllables in speech. In nfPPA patients, its atrophy is associated with the severity of speech impairment based on the Apraxia of Speech Rating Scale [13]. Focal atrophy of the left superior lateral premotor cortex is associated with PPAS. PPAS conversion to nfPPA is attributed to atrophy involving the left inferior frontal gyrus and subcortical structures [11, 16]. Some studies show that atrophy of the regions associated with agrammatism occurs before its clinical manifestation and may predict which proportion of PPAS patients will progress to nfPPA over time.
In addition to apraxia of speech, patients with PPAS and nfPPA develop nonverbal oral apraxia. In this type of apraxia, people are unable to consciously purse their lips, blow, or cough. In nfPPA and PPAS, nonverbal oral apraxia is associated with bilateral involvement of prefrontal and premotor cortex and SMA [17]. Ideomotor apraxia, which is common in nfPPA, is also associated with left premotor cortex atrophy [18].
Predominant damage to certain regions and the connections between them appear to explain the clinical heterogeneity of nfPPA; for example, predominant damage to the motor component is reported in premotor cortex atrophy and agrammatism in prefrontal cortex degeneration, whereas simultaneous damage to all regions results in early mutism [19–22].
Genetic variants of nfPPA may differ from sporadic variants in the pattern of atrophy. A small study showed that nfPPA patients with GRN mutations had a more posterior pattern of atrophy with bilateral involvement of the lateral parietal lobe, less involvement of the left frontal lobe, and more extensive atrophy of the frontoinsular regions of the right hemisphere [23].
In addition to grey matter, nfPPA also involves degeneration of white fibers connecting the frontal lobes, subcortical structures, and parietal regions. Atrophy is shown to progress from the inferior frontal gyrus to the SMA via the frontal oblique fasciculus. The severity of its damage is associated with the severity of apraxia of speech [24], as well as with impaired speech fluency, while damage to the arcuate and superior longitudinal fasciculi is associated with impaired syntactic structure of speech [25, 26].
Semantic variant
Compared to other variants of PPA, svPPA is characterized by the greatest clinical, pathomorphological, genetic, and neuroimaging homogeneity. Anomia and impaired semantic knowledge of objects are the main clinical features of svPPA. In addition, patients may have dyslexia, dysgraphia, and impaired object knowledge. However, fluency and repetition are spared [1]. The atrophy affects the temporal pole, usually the left one (Figure, В). However, in about one-third of cases, atrophy of the right hemisphere predominates, with more severe behavioral disturbances and prosopagnosia in the clinical picture [6]. Pathological studies show that the vast majority of svPPA patients have a frontotemporal degeneration with an abnormal accumulation of TDP-43 type C [5, 6]. Cases with TDP-43 type A or B, tauopathy, or Alzheimer's degeneration are less common. Hereditary forms are less typical for svPPA than for nfPPA. Genetic mutations are found in approximately 2–4% of cases, a positive family history is reported in 2–17% of patients, and most cases are sporadic [27, 28].
Although naming disorders are present in all variants of PPA, they are most severe in svPPA patients. The diagnosis of svPPA should consider that at early stages, knowledge of less common concepts and objects may be impaired, while knowledge of more familiar and general concepts may be spared. As svPPA progresses, the comprehension of familiar and routine words is also impaired. Patients often tend to replace rare words with familiar terms (e.g., they may say an animal when presented with a picture of a giraffe) or use nonspecific words (this, thing, something). In contrast to nfPPA, nouns present the greatest difficulty. Since the anomia is based on a loss of word knowledge, a choice of 4 prompt words usually does not help patients with naming tests, in contrast to other PPA variants. In addition to verbal deficits, patients also have impaired ability to perform nonverbal semantic tasks such as identifying colors, sounds, smells, celebrity faces, and object functions, suggesting a widespread loss of semantic knowledge in this variant [29–31]. In addition to anomia, patients may have mild dysgraphia and dyslexia, manifested by misspelled words or unpronounceable consonants. In contrast, impaired repetition, syntax, or grammar are not typical for svPPA, and sentence comprehension is usually better than that of single words (due to additional context).
Despite severe semantic deficit, episodic and autobiographical memory are usually spared or relatively spared, although they are often difficult to test because of language and speech disorders. Behavioral disturbances are more typical for svPPA than for other variants, occur earlier, and are more severe [6]. Disinhibition, egocentrism, loss of empathy for close ones, compulsive behavior, and personality changes are frequently observed. Reduced insight is often reported.
In most cases, svPPA begins with atrophy of the left temporal pole [1], which is a semantic hub for storing, processing, and retrieving verbal semantic information. Interestingly, the study of svPPA has greatly aided in the identification of this function of the left temporal pole. Structural and functional neuroimaging data showed that disruption of multiple connections of the left temporal pole with regions of the semantic evaluation network and other cortical regions is associated with anomia and impaired single word comprehension due to semantic deficit, and that left temporal pole atrophy correlates with the severity of naming disorders [32–34].
As noted above, approximately 30% of svPPA patients have atrophy that develops from the right rather than the left temporal pole [32]. In this case, the first symptoms include non-verbal semantic impairment, such as the inability to recognize familiar faces, images, and objects [35], since the right temporal pole is responsible for encoding predominantly non-verbal semantic stimuli and contributes to recognizing familiar visual images [36]. In addition, verbal semantic functions may be spared in such patients at the early stages of the disease, or such disorders may be less severe than in those with left-sided onset of the disease. Right-sided svPPA is characterized by more severe and earlier behavioral disturbances, which may complicate differential diagnosis with the behavioral variant of frontotemporal dementia. This is because the right temporal pole and right fusiform gyrus play an important role in the perception of emotions, empathy, and recognition of familiar faces [29, 37, 38], and atrophy of the right fusiform gyrus, the right inferior temporal gyrus, and bilateral atrophy of the temporal poles and amygdalae correlate with the impaired model of perception of other mind [39].
As the disease progresses, the atrophy of the temporal poles becomes more symmetrical, leading to a decrease in differences in clinical manifestations between different forms of svPPA. Left-sided svPPA gradually presents with behavioral and non-verbal semantic deficits, and right-sided svPPA develops language and speech disorders [32, 40]. In addition to contralateral progression, atrophy also affects regions associated with the anterior temporal pole, extending to more posterior parts of the temporal lobe and orbitofrontal areas [41]. Damage to the middle parts of the left superior and middle temporal gyri in svPPA, which are thought to be responsible for connecting semantic regions with parietal and posterior temporal regions, correlates with the severity of anomia, impaired single word comprehension, and dyslexia [32, 33]. Moreover, svPPA is characterized by atrophy of the hippocampus and parahippocampal gyri [4], which may complicate the differential diagnosis with AD. However, in contrast to the latter, hippocampal atrophy is asymmetric and predominantly affects anterior rather than posterior regions [42]. In addition to the right temporal lobe, other brain regions are involved in the development of emotional disturbances in svPPA. Impaired emotion recognition correlates with atrophy of the orbitofrontal cortex, which is normally involved in processing emotional information from the temporal poles and regulating complex social behavior [38]. In addition to the right temporal lobe and orbitofrontal cortex, the decline in emotional memory also correlates with decreased volume of the right frontal pole [43]. Structural abnormalities are not restricted to the grey matter of the brain, as in nfPPA. In svPPA, lesions are found in the ventral white matter tracts of the frontotemporal regions, usually the anterior part of the inferior longitudinal fasciculi and uncinate fasciculi [25, 44].
Logopenic variant
Key features of lvPPA include impaired word selection in spontaneous speech and naming, and impaired repetition of long phrases and sentences, while the motor component of speech and semantic knowledge are spared and no agrammatism is observed [45]. In addition, phonological speech errors are typical for lvPPA. Histologically, in contrast to the other two variants, the vast majority of lvPPA patients have Alzheimer's degeneration; less frequently (in 5–40% of cases), variants of frontotemporal degeneration with accumulation of tau protein or TDP-43 can be observed [5, 46–48]. In lvPPA associated with frontotemporal degeneration, hereditary forms can also occur, most commonly with mutations in the GRN gene [49, 50].
Although naming disorders are important clinical manifestations of both svPPA and lvPPA, their underlying mechanisms are very different. Anomia and impaired repetition of long phrases in lvPPA develop as a result of atrophy of other brain regions such as posterior parts of the temporal lobes, middle temporal gyrus, angular gyrus and the precuneus of the left hemisphere [51, 52]. This is because semantic information is transmitted from the anterior temporal pole to the left temporoparietal junction, where it is re-coded into phonological form and sent to the motor speech areas of the frontal lobes. This region is also responsible for short-term phonological storage (i.e., the “phonological loop”) [53]. Therefore, despite the presence of anomia due to the disrupted connection between motor and semantic language areas, in lvPPA, unlike svPPA, single word comprehension is spared and no atrophy is observed in the left temporal pole responsible for the storage of verbal semantic information [52]. Impaired phonological memory leads to the main clinical manifestations of lvPPA, such as speech pauses when searching for words, phonological paraphasias when naming words (especially long ones), difficulty repeating long unfamiliar sentences or a series of numbers or words. However, repetition of single words or short phrases is usually unaffected or less affected.
Differential diagnosis between lvPPA and nfPPA tends to be the most difficult because of the similarity in clinical presentation (impaired fluency, pronunciation errors). Speech pauses in lvPPA are caused by difficulty finding words and alternate with fluent speech. Speech production rate is moderately reduced, not markedly as in nfPPA; patients can replace a forgotten word with its description; and they are well helped by prompts to the first syllable of the word, both in oral speech and in naming tasks [45, 54]. Sound errors in lvPPA consist mainly of substitution, deletion, or insertion of single existing phonemes, whereas in nfPPA they are phonetic, with initial mispronunciation of sounds [55]. As with nfPPA, there may be a slight decrease in the understanding of complex syntactic structures, but this is due to impaired phonological storage rather than a lack of understanding of grammatical structures [56]. Some studies suggest that difficulties in the diagnosis of lvPPA and in the differential diagnosis between lvPPA and nfPPA are due to drawbacks of existing diagnostic criteria [57, 58]. For example, nfPPA patients without apraxia of speech may meet the core criteria for both nfPPA and lvPPA. In this regard, it is proposed to slightly modify the existing criteria so that one of the mandatory signs of lvPPA would be the lack of agrammatism and language comprehension disorders [59]. Other researchers point to the lack of sensitivity of the criteria at the early stages and suggest to make them less stringent, allowing for some difficulty with single word comprehension and emphasizing the absence of any decline in fluency, except for isolated pauses for searching for words [60].
In addition to aphasia, lvPPA is characterized by mild to moderate non-verbal cognitive impairment, such as visuospatial impairment, dyscalculia, executive function and memory impairment, which may be primarily due to Alzheimer's degeneration [61–63]. Over time, global aphasia with significant impairment of other cognitive functions is common and, in the absence of a medical history, differential diagnosis with the amnestic variant of AD may be challenging [56, 62, 64]. Slow progression is less common, with minimal increase in symptoms and grey matter atrophy [65].
In lvPPA, various behavioral disturbances may also develop, although they are less severe than in svPPA and nfPPA. Anxiety, irritability, depression, and apathy are more typical, while disinhibition or decreased empathy are less common [10, 66]. Some studies show that behavioral disturbances in lvPPA occur only at the late stages, when the severity of aphasia reaches a high level [67].
LvPPA is characterized by atrophy of the left posterior perisylvian and parietal regions such as the inferior parietal lobule, the temporoparietal junction, and the posterior parts of the temporal lobe (Figure, С), which play an important role in phonological storage [1]. Over time, atrophy may progress to the frontal areas of the brain and the hippocampus, which is associated with additional symptoms of other variants of PPA [68]. The pattern of atrophy also seems to depend on the pathomorphological variant of the disease. In one of the studies, atrophy was more severe in lvPPA with positive AD markers compared with lvPPA without AD markers in the left superior parietal region, inferior temporal gyrus, and more ventral parts of the superior and middle temporal gyri [46]. In general, less studies have been performed to evaluate neuroimaging markers of lvPPA compared with other variants because lvPPA is often considered together with other variants of AD without focusing on language disorders. Available studies of clinical and neuroimaging correlations have shown that naming disorders are associated with atrophy of the middle parts of the left temporal gyrus [33, 52], repetition disorders correlate with damage to the left angular, supramarginal gyri, and posterior parts of the superior temporal gyrus [51], and the rate of phonological speech errors increases with the severity of atrophy of the supramarginal gyrus and inferior parietal lobule [69]. In lvPPA, white matter damage is less severe than in nfPPA and svPPA, affecting only the temporoparietal regions [25].
Conclusion
Different variants of PPA represent a unique model to study speech function because their clinical diversity affects almost all speech domains. The selectivity of focal network damage allows a more precise determination of the structures and functionally related regions involved in different aspects of speech. Current insights on the function of the language network not only contribute to fundamental ideas about how information is processed in the central nervous system, but also have immediate practical implications. A deep understanding of the neuroanatomy of language and speech is necessary to perform neurosurgical procedures in functionally significant regions, such as tumor removal. The network model of language can also be used to rehabilitate aphasic patients by selecting the optimal target for navigated transcranial magnetic stimulation or transcranial direct current stimulation. Despite significant advances in the understanding of the neuroanatomy of language in recent years, further comprehensive studies of the language network using the latest neuroimaging and neurophysiological techniques are needed to identify alternative compensatory options for patients with language disorders.
About the authors
Diliara R. Akhmadullina
Research Center of Neurology
Email: fedotova@neurology.ru
ORCID iD: 0000-0001-6491-2891
postgraduate student
Russian Federation, MoscowEkaterina Y. Fedotova
Research Center of Neurology
Author for correspondence.
Email: fedotova@neurology.ru
ORCID iD: 0000-0001-8070-7644
Dr. Sci. (Med.), leading researcher, Head, 5th Neurology department, Institute of Clinical and Preventive Neurology
Russian Federation, MoscowReferences
- Gorno-Tempini M.L., Hillis A.E., Weintraub S. et al. Classification of primary progressive aphasia and its variants. Neurology. 2011;76(11):1006–1014. doi: 10.1212/WNL.0b013e31821103e6
- Pick A. Über die Beziehungen der senilen Atrophie zur Aphasie. Prager Medizinische Wochenschrift. 1892;17:165–167.
- Mesulam M. Primary progressive aphasia — differentiation from Alzheimer’s disease. Ann. Neurol. 1987;22(4):533–534. doi: 10.1002/ana.410220414
- Gordon E., Rohrer J.D., Fox N.C. Advances in neuroimaging in frontotemporal dementia. J. Neurochem. 2016;138(Suppl 1):193–210. doi: 10.1111/jnc.13656
- Bergeron D., Gorno‐Tempini M.L., Rabinovici G.D. et al. Prevalence of amyloid‐β pathology in distinct variants of primary progressive aphasia. Ann. Neurol. 2018;84(5):729–740. doi: 10.1002/ana.25333
- Botha H., Josephs K.A. Primary progressive aphasias and apraxia of speech. Continuum (Minneap Minn). 2019;25(1):101–127. doi: 10.1212/CON.0000000000000699
- Ash S., Moore P., Vesely L. et al. Non-fluent speech in frontotemporal lobar degeneration. J. Neurolinguistics. 2009;22(4):370–383. doi: 10.1016/j.jneuroling.2008.12.001
- Tippett D.C., Keser Z. Clinical and neuroimaging characteristics of primary progressive aphasia. Handb. Clin. Neurol. 2022;185:81–97. doi: 10.1016/B978-0-12-823384-9.00016-5
- Butts A.M., Machulda M.M., Duffy J.R. et al. Neuropsychological profiles differ among the three variants of primary progressive aphasia. J. Int. Neuropsychol. Soc. 2015;21(6):429–435. doi: 10.1017/S1355617715000399
- Rohrer J.D., Warren J.D. Phenomenology and anatomy of abnormal behaviours in primary progressive aphasia. J. Neurol. Sci. 2010;293(1–2):35–38. doi: 10.1016/j.jns.2010.03.012
- Whitwell J.L., Duffy J.R., Machulda M.M. et al. Tracking the development of agrammatic aphasia: a tensor-based morphometry study. Cortex. 2017;90:138–148. doi: 10.1016/j.cortex.2016.09.017
- Tetzloff K.A., Utianski R.L., Duffy J.R. et al. Quantitative analysis of agrammatism in agrammatic primary progressive aphasia and dominant apraxia of speech. J. Speech Lang. Hear. Res. 2018;61(9):2337–2346. doi: 10.1044/2018_JSLHR-L-17-0474
- Whitwell J.L., Duffy J.R., Strand E.A. et al. Distinct regional anatomic and functional correlates of neurodegenerative apraxia of speech and aphasia: an MRI and FDG-PET study. Brain Lang. 2013;125(3):245–252. doi: 10.1016/j.bandl.2013.02.005
- Mandelli M.L., Vitali P., Santos M. et al. Two insular regions are differentially involved in behavioral variant FTD and nonfluent/agrammatic variant PPA. Cortex. 2016;74:149–157. doi: 10.1016/j.cortex.2015.10.012
- Cordella C., Quimby M., Touroutoglou A. et al. Quantification of motor speech impairment and its anatomic basis in primary progressive aphasia. Neurology. 2019;92(17):e1992–e2004. doi: 10.1212/WNL.0000000000007367
- Josephs K.A., Duffy J.R., Strand E.A. et al. The evolution of primary progressive apraxia of speech. Brain. 2014;137(Pt 10):2783–2795. doi: 10.1093/brain/awu223
- Botha H., Duffy J.R., Strand E.A. et al. Nonverbal oral apraxia in primary progressive aphasia and apraxia of speech. Neurology. 2014;82(19):1729–1735. doi: 10.1212/WNL.0000000000000412
- Adeli A., Whitwell J.L., Duffy J.R. et al. Ideomotor apraxia in agrammatic and logopenic variants of primary progressive aphasia. J. Neurol. 2013;260(6):1594–1600. doi: 10.1007/s00415-013-6839-9
- Tetzloff K.A., Duffy J.R., Clark H.M. et al. Longitudinal structural and molecular neuroimaging in agrammatic primary progressive aphasia. Brain. 2018;141(1):302–317. doi: 10.1093/brain/awx293
- Josephs K.A., Duffy J.R., Strand E.A. et al. Characterizing a neurodegenerative syndrome: primary progressive apraxia of speech. Brain. 2012;135(Pt 5):1522–1536. doi: 10.1093/brain/aws032
- Mandelli M.L., Welch A.E., Vilaplana E. et al. Altered topology of the functional speech production network in non-fluent/agrammatic variant of PPA. Cortex. 2018;108:252–264. doi: 10.1016/j.cortex.2018.08.002
- Gorno-Tempini M.L., Ogar J.M., Brambati S.M. et al. Anatomical correlates of early mutism in progressive nonfluent aphasia. Neurology. 2006;67(10):1849–1851. doi: 10.1212/01.wnl.0000237038.55627.5b
- Samra K., MacDougall A.M., Bouzigues A. et al. Genetic forms of primary progressive aphasia within the GENetic Frontotemporal dementia Initiative (GENFI) cohort: comparison with sporadic primary progressive aphasia. Brain Commun. 2023;5(2):fcad036. doi: 10.1093/braincomms/fcad036
- Dick A.S., Garic D., Graziano P., Tremblay P. The frontal aslant tract (FAT) and its role in speech, language and executive function. Cortex. 2019;111:148–163. doi: 10.1016/j.cortex.2018.10.015
- Galantucci S., Tartaglia M.C., Wilson S.M. et al. White matter damage in primary progressive aphasias: a diffusion tensor tractography study. Brain. 2011;134(Pt 10):3011–3029. doi: 10.1093/brain/awr099
- Mandelli M.L., Vilaplana E., Brown J.A. et al. Healthy brain connectivity predicts atrophy progression in non-fluent variant of primary progressive aphasia. Brain. 2016;139(Pt 10):2778–2791. doi: 10.1093/brain/aww195
- Goldman J.S., Farmer J.M., Wood E.M. et al. Comparison of family histories in FTLD subtypes and related tauopathies. Neurology. 2005;65(11):1817–1819. doi: 10.1212/01.wnl.0000187068.92184.63
- Seelaar H., Kamphorst W., Rosso S.M. et al. Distinct genetic forms of frontotemporal dementia. Neurology. 2008;71(16):1220–1226. doi: 10.1212/01.wnl.0000319702.37497.72
- Luzzi S., Baldinelli S., Ranaldi V. et al. Famous faces and voices: differential profiles in early right and left semantic dementia and in Alzheimer’s disease. Neuropsychologia. 2017;94:118–128. doi: 10.1016/j.neuropsychologia.2016.11.020
- Luzzi S., Snowden J.S., Neary D. et al. Distinct patterns of olfactory impairment in Alzheimer’s disease, semantic dementia, frontotemporal dementia, and corticobasal degeneration. Neuropsychologia. 2007;45(8):1823–1831. doi: 10.1016/j.neuropsychologia.2006.12.008
- Goll J.C., Crutch S.J., Loo J.H.Y. et al. Non-verbal sound processing in the primary progressive aphasias. Brain. 2010;133(Pt 1):272–285. doi: 10.1093/brain/awp235
- Binney R.J., Henry M.L., Babiak M. et al. Reading words and other people: a comparison of exception word, familiar face and affect processing in the left and right temporal variants of primary progressive aphasia. Cortex. 2016;82:147–163. doi: 10.1016/j.cortex.2016.05.014
- Migliaccio R., Boutet C., Valabregue R. et al. The brain network of naming: a lesson from primary progressive aphasia. PLoS One. 2016;11(2):e0148707. doi: 10.1371/journal.pone.0148707
- Agosta F., Galantucci S., Valsasina P. et al. Disrupted brain connectome in semantic variant of primary progressive aphasia. Neurobiol. Aging. 2014;35(11):2646–2655. doi: 10.1016/j.neurobiolaging.2014.05.017
- Snowden J.S., Harris J.M., Thompson J.C. et al. Semantic dementia and the left and right temporal lobes. Cortex. 2018;107:188–203. doi: 10.1016/j.cortex.2017.08.024
- Borghesani V., Narvid J., Battistella G. et al. “Looks familiar, but I do not know who she is”: the role of the anterior right temporal lobe in famous face recognition. Cortex. 2019;115:72–85. doi: 10.1016/j.cortex.2019.01.006
- Fittipaldi S., Ibanez A., Baez S. et al. More than words: social cognition across variants of primary progressive aphasia. Neurosci. Biobehav. Rev. 2019;100:263–284. doi: 10.1016/j.neubiorev.2019.02.020
- Kumfor F., Landin-Romero R., Devenney E. et al. On the right side? A longitudinal study of left-versus right-lateralized semantic dementia. Brain. 2016;139(Pt 3):986–998. doi: 10.1093/brain/awv387
- Irish M., Hodges J.R., Piguet O. Right anterior temporal lobe dysfunction underlies theory of mind impairments in semantic dementia. Brain. 2014;137(Pt 4):1241–1253. doi: 10.1093/brain/awu003
- Brambati S.M., Amici S., Racine C.A. et al. Longitudinal gray matter contraction in three variants of primary progressive aphasia: a tenser-based morphometry study. Neuroimage Clin. 2015;8:345–355. doi: 10.1016/j.nicl.2015.01.011
- Brambati S.M., Rankin K.P., Narvid J. et al. Atrophy progression in semantic dementia with asymmetric temporal involvement: a tensor-based morphometry study. Neurobiol. Aging. 2009;30(1):103–111. doi: 10.1016/j.neurobiolaging.2007.05.014
- Wisse L.E.M., Ungrady M.B., Ittyerah R. et al. Cross-sectional and longitudinal medial temporal lobe subregional atrophy patterns in semantic variant primary progressive aphasia. Neurobiol. Aging. 2021;98:231–241. doi: 10.1016/j.neurobiolaging.2020.11.012
- Kumfor F., Irish M., Hodges J.R., Piguet O. The orbitofrontal cortex is involved in emotional enhancement of memory: evidence from the dementias. Brain. 2013;136(Pt 10):2992–3003. doi: 10.1093/brain/awt185
- Agosta F., Henry R.G., Migliaccio R. et al. Language networks in semantic dementia. Brain. 2010;133(Pt 1):286–299. doi: 10.1093/brain/awp233
- Mendez M.F. Early-onset Alzheimer disease and its variants. Continuum (Minneap. Minn.). 2019;25(1):34–51. doi: 10.1212/CON.0000000000000687
- Teichmann M., Kas A., Boutet C. et al. Deciphering logopenic primary progressive aphasia: a clinical, imaging and biomarker investigation. Brain. 2013;136(Pt 11):3474–3488. doi: 10.1093/brain/awt266
- Montembeault M., Brambati S.M., Gorno-Tempini M.L. Clinical, anatomical, and pathological features in the three variants of primary progressive aphasia: a review. Front. Neurol. 2018;9:692. doi: 10.3389/fneur.2018.00692
- Magnin E., Démonet J.F., Wallon D. et al. Primary progressive aphasia in the Network of French Alzheimer Plan Memory Centers. J. Alzheimers Dis. 2016;54(4):1459–1471. doi: 10.3233/JAD-160536
- Saracino D., Ferrieux S., Noguès-Lassiaille M. et al. Primary progressive aphasia associated with GRN mutations. Neurology. 2021;97(1):e88–e102. doi: 10.1212/WNL.0000000000012174
- Ramos E.M., Dokuru D.R., Van Berlo V. et al. Genetic screen in a large series of patients with primary progressive aphasia. Alzheimers Dement. 2019;15(4):553–560. doi: 10.1016/j.jalz.2018.10.009
- Lukic S., Mandelli M.L., Welch A. et al. Neurocognitive basis of repetition deficits in primary progressive aphasia. Brain Lang. 2019;194:35–45. doi: 10.1016/j.bandl.2019.04.003
- Win K.T., Pluta J., Yushkevich P. et al. Neural correlates of verbal episodic memory and lexical retrieval in logopenic variant primary progressive aphasia. Front. Neurosci. 2017;11:330. doi: 10.3389/fnins.2017.00330
- Henry M.L., Wilson S.M., Babiak M.C. et al. Phonological processing in primary progressive aphasia. J. Cogn. Neurosci. 2016;28(2):210–222. doi: 10.1162/jocn_a_00901
- Wilson S.M., Henry M.L., Besbris M. et al. Connected speech production in three variants of primary progressive aphasia. Brain. 2010;133(Pt 7):2069–2088. doi: 10.1093/brain/awq129
- Dalton S.G.H., Shultz C., Henry M.L. et al. Describing phonological paraphasias in three variants of primary progressive aphasia. Am. J. Speech Lang. Pathol. 2018;27(1S):336–349. doi: 10.1044/2017_AJSLP-16-0210
- Gorno-Tempini M.L., Brambati S.M., Ginex V. et al. The logopenic/phonological variant of primary progressive aphasia. Neurology. 2008;71(16):1227–1234. doi: 10.1212/01.wnl.0000320506.79811.da
- Wicklund M.R., Duffy J.R., Strand E.A. et al. Quantitative application of the primary progressive aphasia consensus criteria. Neurology. 2014;82(13):1119–1126. doi: 10.1212/WNL.0000000000000261
- Harris J.M., Gall C., Thompson J.C. et al. Classification and pathology of primary progressive aphasia. Neurology. 2013;81(21):1832–1839. doi: 10.1212/01.wnl.0000436070.28137.7b
- Mesulam M.M., Weintraub S. Is it time to revisit the classification guidelines for primary progressive aphasia? Neurology. 2014;82(13):1108–1109. doi: 10.1212/WNL.0000000000000272
- Botha H., Duffy J.R., Whitwell J.L. et al. Classification and clinicoradiologic features of primary progressive aphasia (PPA) and apraxia of speech. Cortex. 2015;69:220–236. doi: 10.1016/j.cortex.2015.05.013
- Leyton C.E., Hsieh S., Mioshi E. Cognitive decline in logopenic aphasia: more than losing words. Neurology. 2013;80(10):897–903. doi: 10.1212/WNL.0b013e318285c15b
- Watson C.L., Possin K., Allen I.E. et al. Visuospatial functioning in the primary progressive aphasias. J. Int. Neuropsychol. Soc. 2018;24(3):259–268. doi: 10.1017/S1355617717000984
- Tippett D.C., Breining B., Goldberg E. et al. Visuomotor figure construction and visual figure delayed recall and recognition in primary progressive aphasia. Aphasiology. 2020;34(12):1456–1470. doi: 10.1080/02687038.2019.1670330
- Rohrer J.D., Caso F., Mahoney C. et al. Patterns of longitudinal brain atrophy in the logopenic variant of primary progressive aphasia. Brain Lang. 2013;127(2):121–126. doi: 10.1016/j.bandl.2012.12.008
- Machulda M.M., Whitwell J.L., Duffy J.R. et al. Identification of an atypical variant of logopenic progressive aphasia. Brain Lang. 2013;127(2):139–144. doi: 10.1016/j.bandl.2013.02.007
- Van Langenhove T., Leyton C.E., Piguet O., Hodges J.R. Comparing longitudinal behavior changes in the primary progressive aphasias. J. Alzheimers Dis. 2016;53(3):1033–1042. doi: 10.3233/JAD-160010
- Keator L.M., Wright A.E., Saxena S. et al. Distinguishing logopenic from semantic and nonfluent variant primary progressive aphasia: patterns of linguistic and behavioral correlations. Neurocase. 2019;25(3–4):98–105. doi: 10.1080/13554794.2019.1625929
- Rogalski E., Cobia D., Harrison T.M. et al. Progression of language decline and cortical atrophy in subtypes of primary progressive aphasia. Neurology. 2011;76(21):1804–1810. doi: 10.1212/WNL.0b013e31821ccd3c
- Petroi D., Duffy J.R., Borgert A. et al. Neuroanatomical correlates of phonologic errors in logopenic progressive aphasia. Brain Lang. 2020;204:104773. doi: 10.1016/j.bandl.2020.104773